Root canal treatment is a dental procedure that involves removing the infected pulp from a tooth to save it from extraction. The procedure typically consists of three stages: the diagnosis and preparation stage, the cleaning and shaping stage, and the filling and sealing stage.
1. Diagnosis and Preparation Stage:
The first stage of root canal treatment involves diagnosing the need for the procedure. This is done by the dentist through a thorough examination, often with the help of dental X-rays. The dentist will check for signs of infection, such as tooth pain, sensitivity to hot or cold temperatures, swelling, or abscesses. Once the need for root canal treatment is established, the dentist will prepare the patient for the procedure. This includes explaining the process, potential risks, and benefits. Local anesthesia is usually administered to numb the area around the tooth to ensure a pain-free experience for the patient.
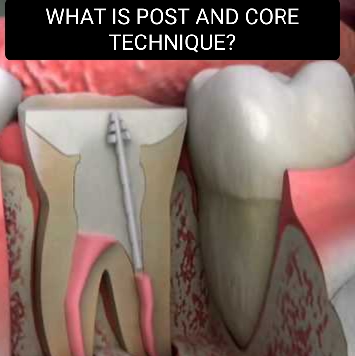
The first stage of root canal treatment (RCT) is the access opening. This step involves creating an opening in the tooth to gain access to the root canal system where the infected or inflamed pulp is located. Here is a detailed explanation of the access opening stage:
1. Anesthesia:
Before beginning the procedure, the dentist will administer local anesthesia to numb the tooth and surrounding area, ensuring a comfortable and pain-free experience for the patient.
2. Isolation:
The dentist will use a dental dam, a thin rubber sheet, to isolate the tooth being treated. The dental dam helps to keep the area clean and dry during the procedure, preventing saliva or other contaminants from entering the tooth.
3. Tooth Preparation:
The dentist will prepare the tooth by removing any decayed or damaged areas of the tooth structure. This is crucial to ensure a clear path to the root canals and facilitate the subsequent stages of the treatment.
4. Drilling:
Using a dental drill or other appropriate instruments, the dentist will create a small opening in the crown of the tooth. The access opening can vary in size and shape depending on the specific tooth being treated and the accessibility required for adequate cleaning and shaping of the root canals.
5. Pulp Chamber Exposure:
Once the access opening is created, the dentist will carefully remove any remaining decayed or infected dental pulp from the pulp chamber, which is the hollow space in the center of the tooth that contains the nerve tissue. This step helps to relieve pain and eliminate the source of infection.
6. Canal Identification:
The dentist will locate the entrance to the root canals within the pulp chamber. Each tooth has a varying number of root canals depending on its anatomy. The dentist will use dental instruments and an operating microscope, if necessary, to accurately identify and locate the canals. X-rays may also be used to aid in this process.
7. Initial Canal Exploration:
With the entrance of the root canals identified, the dentist will begin the initial exploration of the canals using small, flexible files. These files are inserted into the canals to remove any obstructions, debris, or remnants of the infected pulp.
The access opening stage provides the dentist with direct access to the root canal system for effective cleaning, disinfection, and subsequent shaping. Once the access opening is complete, the dentist will proceed to the next stages of RCT, including cleaning and shaping the canals and filling them with a root canal filling material.
2. Cleaning and Shaping Stage:
In this stage, the dentist starts by creating a small access hole in the tooth. This access hole allows them to reach the pulp chamber and root canals. Specialized instruments, including small files and drills, are used to carefully remove the infected or inflamed pulp tissue from the tooth.
The dentist then cleans the canals thoroughly to remove any remaining infected material or bacteria. This is achieved by using antibacterial irrigating solutions and small brushes to ensure the canals are clean and disinfected. Additionally, the dentist may use special instruments to shape the inside of the canals to facilitate effective filling in the next stage.
The second stage of root canal treatment (RCT) is Biomechanical Preparation. After the access opening is made, this stage involves the cleaning and shaping of the root canals to remove any remaining infected or inflamed pulp, debris, and bacteria. Here is a detailed explanation of the biomechanical preparation stage:
1. Canal Irrigation:
The dentist will first use an irrigating solution, typically a sodium hypochlorite solution, to flush and disinfect the root canals. Irrigation helps in removing debris, dissolving organic material, and killing bacteria that may be present in the canals.
2. Determining Working Length:
The dentist will determine the working length of each root canal. This involves measuring the length of the canal from the access opening to the tip of the root by using X-rays or an electronic apex locator. Knowing the proper working length is important for accurate cleaning and filling of the canals.
3. Canal Shaping:
Once the working length is determined, the dentist will use specialized dental instruments called files to shape the canals. The files are carefully inserted into the canals and rotated to remove the infected tissue and shape the canals to a form that can be easily cleaned and adequately filled.
4. Step-back Technique:
The step-back technique is commonly used in canal shaping. It involves using progressively larger files to gradually shape the canal from the apex to the access opening. The files are tapered and have a cutting edge that helps in removing the infected tissue and enlarging the canal width.
5. Recapitulation:
Throughout the canal shaping process, the dentist will intermittently use smaller files to recapitulate the canals. Recapitulation involves reinserting smaller files into the canals to remove any debris or tissue that may have been pushed towards the apex during the shaping process.
6. Canal Irrigation (Again):
After each file, or series of files, is used, the canals are rinsed with an irrigation solution to flush out debris and disinfect the canals. This process is repeated multiple times during the biomechanical preparation stage to ensure thorough cleaning and disinfection.
The biomechanical preparation stage aims to completely clean and shape the root canals, ensuring the removal of infected or inflamed pulp, bacteria, and debris. It establishes a suitable environment for the final stage of RCT, which is the filling of the canals with a root canal filling material to prevent reinfection.
3. Filling and Sealing Stage:
Once the canals are clean and shaped adequately, they are filled and sealed to prevent reinfection. This is typically done in two ways:
– Gutta-percha: A rubber-like material called gutta-percha is used to fill the canals. It is heated and placed into the canals, effectively sealing them and preventing bacteria from reentering. The gutta-percha is often coated with a sealer to enhance the seal.
– Temporary or Permanent Filling: After the canals are filled with gutta-percha, the access hole created at the beginning of the procedure is temporarily sealed with a temporary filling. This allows the tooth to heal before the final step. In some cases, a permanent filling may be placed immediately after the canals are filled, eliminating the need for a temporary filling.
The final stage of root canal treatment (RCT) is sealing or obturation. After the cleaning and shaping of the root canals in the previous stage, the canals need to be sealed to prevent recontamination and to ensure the long-term success of the treatment. Here is a detailed explanation of the sealing stage:
1. Canal Drying:
Before sealing the canals, it is important to ensure that they are thoroughly dried. This is typically done using absorbent paper points that are inserted into the canals to absorb any remaining moisture. The dentist may change the paper points multiple times until the canals are completely dry.
2. Root Canal Sealer:
A root canal sealer is a material used to create a fluid-tight seal inside the canals. It is usually a viscous material that fills the irregularities and gaps between the canal walls and the root canal filling material. The sealer helps to prevent the leakage of bacteria and fluids into the canals.
3. Root Canal Filling Material:
Gutta-percha is the most commonly used material for filling the root canals. Gutta-percha is a rubber-like material that is heated and compacted into the canals, filling the entire space left after the removal of infected pulp and debris. The gutta-percha is often mixed with a root canal sealer to enhance its sealing ability.
4. Obturation Techniques:
There are different techniques used for the placement of gutta-percha in the canals:
– Cold Lateral Condensation: This is one of the most widely used techniques where pre-fitted gutta-percha cones of various sizes are coated with sealer and then compacted laterally using special instruments called spreaders and pluggers. This technique allows for the complete filling of the canal space.
– Warm Gutta-Percha Techniques: In these techniques, the gutta-percha is heated and softened before being placed into the canals. There are different warm gutta-percha techniques, such as the Obtura technique or the System B technique, which use specialized instruments to heat and inject the gutta-percha into the canals.
5. Radiographic Evaluation:
Throughout the sealing stage, X-rays are taken to ensure that the gutta-percha is adequately filling the canals and creating a proper seal. The dentist will assess the radiographs to confirm that the root canal treatment is successful and the canals are fully sealed.
Once the canals are properly sealed and filled, the access opening in the tooth is closed with a permanent filling or a dental restoration. This final stage of sealing in RCT is vital to prevent reinfection and to restore the tooth’s function and integrity.
After the root canal treatment, a crown or dental restoration may be recommended to protect the tooth from further damage or fractures.
It is important to note that the number of stages and specific procedures involved in root canal treatment may differ slightly depending on the complexity of the case and the dentist’s technique. Hence, it’s always best to consult with a dental professional for accurate and detailed information specific to an individual’s case.
UNDERSTANDING THE BENEFITS OF ROOT CANAL TREATMENT
Root canal treatment (RCT) offers several benefits, including:
1. Pain Relief:
RCT is typically performed to alleviate severe tooth pain caused by an infected or inflamed pulp. By removing the damaged tissue and infection, the source of pain is eliminated, providing significant pain relief.
2. Infection Prevention:
RCT removes the infected pulp and thoroughly cleans and disinfects the root canals. This helps to prevent the spread of infection to the surrounding tissues, jawbone, or other teeth.
3. Tooth Preservation:
The primary goal of RCT is to save the natural tooth from extraction. Preserving the natural tooth is crucial for maintaining proper chewing function, speech articulation, and preventing adjacent teeth from shifting into the gap left by extraction. It also helps to maintain the aesthetics of the smile.
4. Restored Functionality:
After RCT, the treated tooth can regain its functionality, allowing you to bite and chew normally. This eliminates any discomfort or limitations in eating that were experienced due to the infected tooth.
5. Protection of Adjacent Teeth:
An infected tooth can potentially spread the infection to neighboring teeth. RCT removes the infection and prevents it from affecting the adjacent healthy teeth, reducing the risk of further dental problems.
6. Longevity:
A properly performed RCT can provide long-lasting results. With proper oral hygiene and regular dental check-ups, a treated tooth can last a lifetime.
7. Aesthetic Appeal:
Following RCT, a dental crown or other restoration is typically placed on the treated tooth to restore its appearance. This helps to maintain a natural, aesthetically pleasing smile.
It is important to note that the success of RCT relies on proper diagnosis, meticulous technique, and adequate restoration of the treated tooth. It is always recommended to consult with a qualified dentist or endodontist to determine if RCT is the best treatment option for your specific dental condition.
WHY IS THERE A NEED OF ROOT CANAL TREATMENT?
Root canal treatment (RCT) is done to save a tooth that has been severely damaged or infected. The need for RCT arises when the pulp, which is the soft tissue inside the tooth that contains nerves, blood vessels, and connective tissues, becomes infected or inflamed. This can occur due to various reasons, including:
1. Decay: When tooth decay is left untreated, it can progress to the pulp, leading to infection and inflammation. The bacteria from the decay can invade the pulp, causing pain, sensitivity, and potentially an abscess.
2. Trauma: A tooth that has experienced a significant impact or injury can develop damage to the pulp. This could be due to a hard blow to the tooth, a sports injury, or a fall.
3. Deep Fillings: Dental fillings that are placed too close to the pulp can irritate the tissue and cause inflammation. Over time, the pulp can become infected, leading to the need for root canal treatment.
4. Cracked or Fractured Tooth: When a tooth is cracked or fractured, the pulp can become exposed or damaged. Bacteria can enter through the fracture, leading to infection and inflammation within the pulp.
CONCLUSION
The primary goal of root canal treatment is to remove the infected or inflamed pulp, clean and disinfect the canals, and then seal them to prevent reinfection. By doing so, the natural tooth can be saved, and the patient can avoid extraction. Preserving the natural tooth is essential for maintaining proper chewing function, speech articulation, and preventing adjacent teeth from shifting into the gap left by extraction.
If left untreated, an infected or damaged tooth can cause severe pain, abscess formation, bone loss, and even systemic health complications. Therefore, root canal treatment is performed to alleviate pain, treat the infection, and restore the tooth’s health and functionality.
RELATED ARTICLE: FREQUENTLY ASKED QUESTIONS FOR RCT